can the immune system fight hiv
HIV, the Human Immunodeficiency Virus, presents a formidable challenge to global health, profoundly affecting the body’s immune system and leading to the development of Acquired Immuno-deficiency Syndrome (AIDS). Despite decades of research and significant progress in treatment options, HIV persists, posing ongoing threats to individuals worldwide.
At the heart of the HIV challenge lies its ability to target and deplete CD4 T cells, crucial defenders of the body’s immune response. This depletion weakens the body’s ability to fight infections and diseases, ultimately leading to the onset of AIDS. Even with powerful antiretroviral therapies, HIV manages to persist within the body, hiding in reservoirs and eluding complete eradication.
Understanding how HIV interacts with the immune system is essential for developing effective strategies to combat the virus. By unraveling this intricate relationship, we can explore new avenues for treatment and potentially even find ways to eliminate HIV altogether. In this article, we’ll explore the dynamic interplay between HIV and the immune system, highlighting the challenges we face, the progress we’ve made, and the possibilities for the future in our ongoing battle against this relentless pathogen.
Understanding HIV and the Immune System:
HIV, or the Human Immunodeficiency Virus, profoundly affects the body’s immune system by specifically targeting a key type of immune cell known as CD4 T cells. These cells play a crucial role in coordinating the body’s defense against infections and diseases.
When HIV enters the bloodstream, it seeks out CD4 T cells, which have a protein called CD4 on their surface. The virus attaches to these CD4 receptors and enters the CD4 T cells, where it hijacks the cell’s machinery to replicate itself. This replication process damages and eventually destroys the CD4 T cells.
The loss of CD4 T cells has significant consequences for the immune system. These cells are essential for organizing the body’s defense against pathogens, including activating other immune cells such as B cells and cytotoxic T cells. As CD4 T cell levels decline, the body becomes more vulnerable to infections and less capable of mounting effective immune responses.
In addition to targeting CD4 T cells, HIV can also infect other immune cells like macrophages and dendritic cells, further weakening the body’s defenses.
As CD4 T cells are progressively depleted, the immune system becomes compromised, leading to immunodeficiency, a characteristic feature of AIDS. Without a functioning immune system, individuals with AIDS become susceptible to a wide range of opportunistic infections and cancers that a healthy immune system would normally control.
HIV undermines the immune system by attacking and reducing CD4 T cells, impairing the body’s ability to mount effective immune responses. Understanding this process is crucial for developing strategies to combat HIV and lessen its devastating impact on the immune system.
The Immune Response to HIV:
When faced with HIV infection, the body’s immune system springs into action, utilizing both innate and adaptive defense mechanisms to combat the virus’s onslaught and limit its spread.
1. Innate Immune Response:
The innate immune system acts as the body’s initial defense against HIV. Key players like dendritic cells, macrophages, and natural killer cells detect the virus and launch a rapid, nonspecific immune reaction. Dendritic cells identify HIV particles and present viral antigens, initiating an inflammatory response. Meanwhile, macrophages engulf and destroy HIV-infected cells, and natural killer cells directly eliminate virus-infected cells.
2. Adaptive Immune Response:
The adaptive immune system orchestrates a more targeted and specific response to HIV, involving specialized immune cells and molecules designed to recognize and eliminate the virus.
a. Cytotoxic T Lymphocytes (CTLs): CTLs, also known as killer T cells, are pivotal in controlling HIV. These immune cells identify specific viral proteins presented on infected cells and eliminate them, restricting viral spread. CTLs are especially effective against HIV-infected cells with high viral replication rates.
b. Neutralizing Antibodies: B cells produce neutralizing antibodies that can bind to and block HIV’s entry into target cells. These antibodies recognize surface proteins on the virus and prevent them from attaching to CD4 receptors on host cells. By neutralizing HIV particles, these antibodies help to curtail viral replication and dissemination.
Challenges to Immune Control:
Despite the immune system’s remarkable capabilities, eliminating HIV presents significant challenges. Several factors contribute to the virus’s ability to evade immune control, prolonging infection and complicating efforts to eradicate it.
1. Evasion of Immune Detection:
HIV employs sophisticated tactics to avoid detection by the immune system. The virus constantly mutates, altering its surface proteins targeted by neutralizing antibodies. These mutations allow HIV to evade recognition, persisting in the body.
Additionally, HIV can downregulate major histocompatibility complex (MHC) molecules on infected cells, reducing visibility to cytotoxic T lymphocytes (CTLs). By hindering immune responses, HIV evades surveillance, enabling unchecked replication.
2. High Mutation Rate:
HIV’s genetic variability poses a challenge to immune control. The virus mutates rapidly due to the error-prone nature of its reverse transcriptase enzyme. This mutation allows HIV to evade immune responses and antiretroviral drugs, leading to drug-resistant strains.
The genetic diversity within an infected individual complicates vaccine and therapy development, as targeting multiple viral strains simultaneously is daunting.
3. Establishment of Viral Reservoirs:
HIV forms latent reservoirs in long-lived cells, where the virus lies dormant and undetectable by the immune system and drugs. These reservoirs, including resting CD4 T cells and tissue macrophages, serve as a persistent viral source.
The presence of viral reservoirs hinders efforts to achieve a functional cure, as complete eradication is challenging. Even with antiretroviral therapy, viral reservoirs persist, impeding sustained remission or eradication.
HIV poses formidable challenges to immune control. Its evasion tactics, mutation rate, and establishment of reservoirs thwart immune responses, perpetuating chronic infection. Overcoming these hurdles requires innovative strategies targeting HIV’s multiple facets, ultimately improving outcomes for those living with HIV/AIDS.
Immune-Evasion Strategies of HIV:
HIV has evolved sophisticated tactics to evade immune surveillance and evade elimination by the host’s immune system. These strategies enable the virus to persist within the body despite the efforts of the immune response. Here are some key mechanisms employed by HIV to evade detection and elimination:
1. Antigenic Variation:
HIV mutates rapidly, leading to frequent changes in its surface proteins, particularly gp120 and gp41. These mutations allow the virus to evade recognition by neutralizing antibodies, facilitating continued replication.
2. Downregulation of Major Histocompatibility Complex (MHC) Molecules:
Infected cells can reduce MHC molecule expression, hindering presentation of viral antigens to cytotoxic T lymphocytes (CTLs). This evasion tactic prevents CTL-mediated destruction of infected cells, allowing HIV to persist.
3. Manipulation of Immune Checkpoints:
HIV can exploit immune checkpoint pathways, like PD-1/PD-L1, to suppress T cell function. Upregulation of PD-L1 on infected cells leads to T cell exhaustion, impairing antiviral immunity.
4. Escape from T Cell Recognition:
HIV may mutate CTL epitopes, evading recognition by CTLs. Additionally, the virus alters antigen processing, reducing CTL recognition and killing efficiency.
5. Resistance to Complement-Mediated Lysis:
HIV resists complement-mediated lysis by acquiring host-derived complement regulatory proteins on its surface, protecting it from complement attack and enhancing its survival.
HIV employs diverse immune-evasion strategies, including antigenic variation, MHC downregulation, immune checkpoint manipulation, T cell recognition evasion, and resistance to complement-mediated lysis. These tactics collectively contribute to HIV persistence and pose challenges for developing effective immune-based therapies and vaccines.
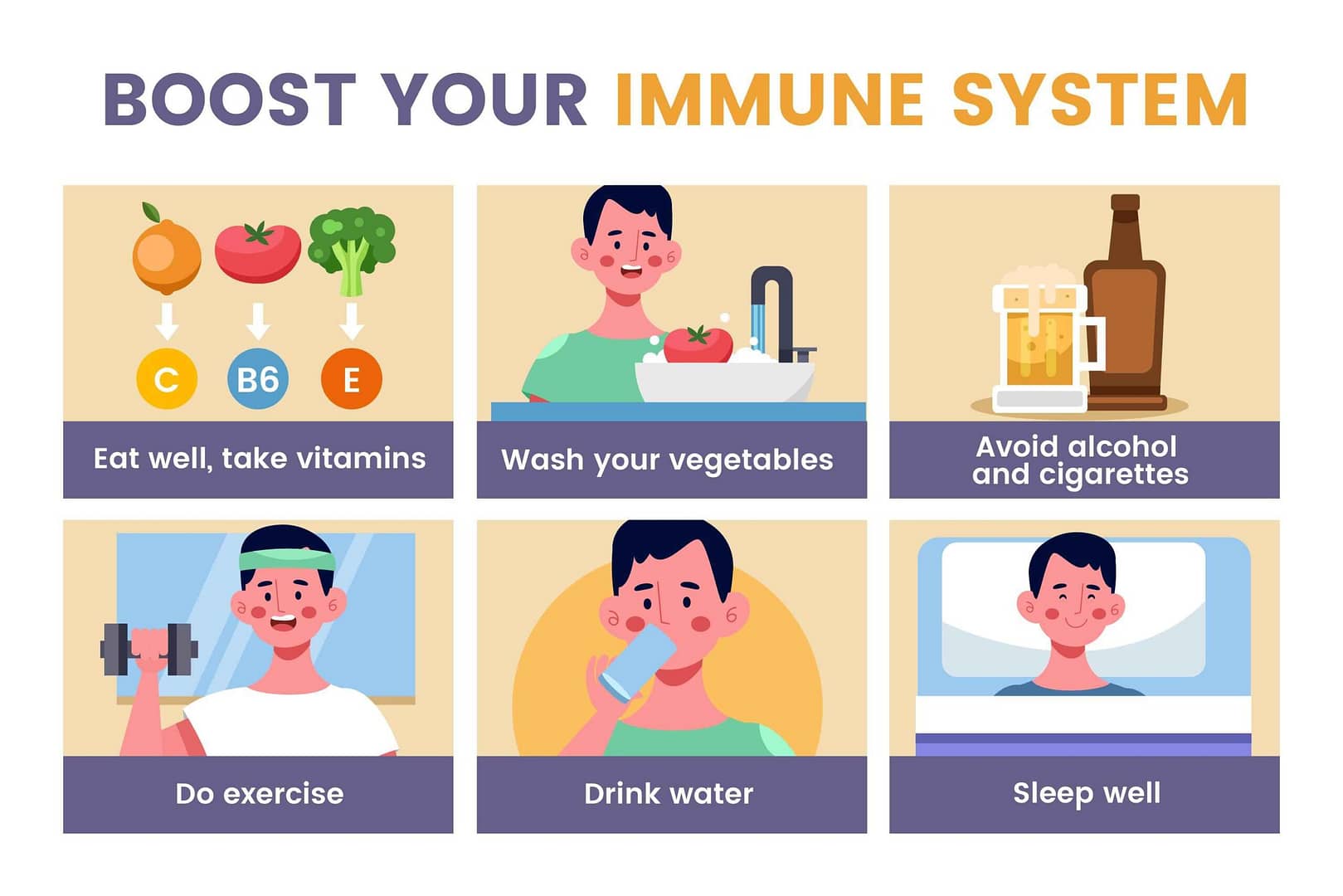
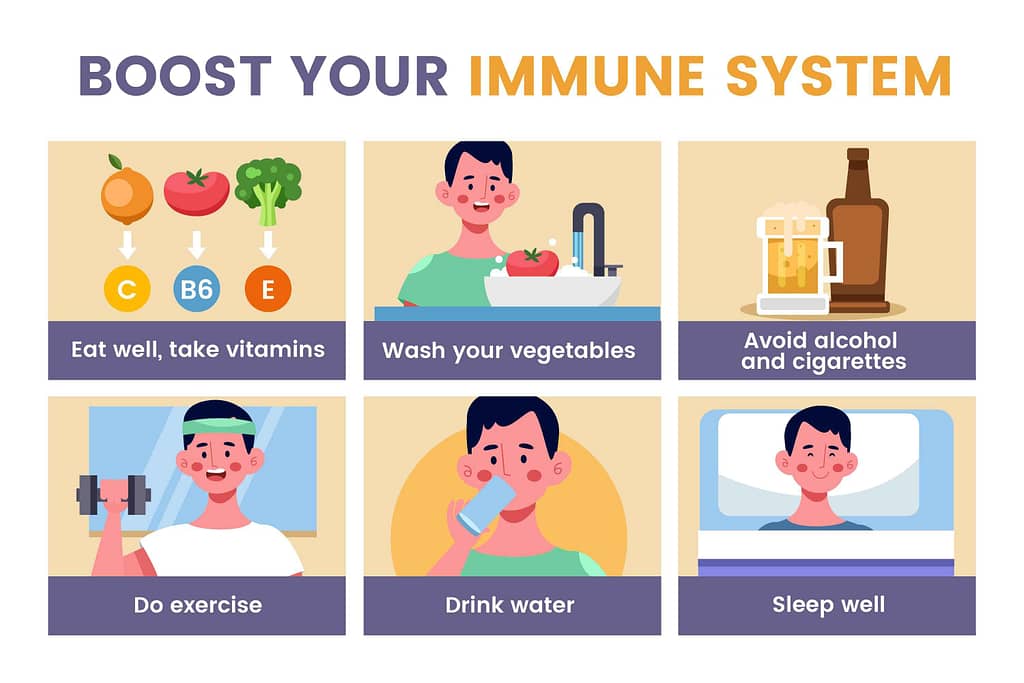
Enhancing Immune Responses Against HIV:
Boosting the body’s ability to fight HIV is crucial for developing effective treatments. Here are some simple strategies being explored:
1. Therapeutic Vaccines:
These vaccines aim to train the immune system to recognize and attack HIV. They’re designed to work in people already infected, helping their immune system fight the virus better.
2. Immuno-modulatory Drugs:
These drugs tweak the immune system to make it better at fighting HIV. Some drugs aim to boost key immune cells, while others help reduce the immune system’s suppression caused by HIV.
3. Broadly Neutralizing Antibodies (bNAbs):
These special antibodies can fight against many different types of HIV. They’re being studied to see if they can be given as treatment or used to help prevent HIV infection.
4. Immune-Based Therapies:
Other treatments involve using the body’s own immune cells to fight HIV. Some methods take immune cells from the patient, boost them in the lab, and then put them back into the patient to fight the virus. Another approach involves changing the genes of immune cells to make them better at fighting HIV.
These strategies are all being researched to find better ways to help the immune system battle HIV and improve the lives of those living with the virus.
Clinical Implications and Future Directions:
Understanding how the immune system interacts with HIV has significant implications for the development of new treatments and vaccines. Here’s a look at what this means for the future of HIV research:
1. Developing Novel Treatments:
Insights into the immune response to HIV can guide the development of innovative treatments. By targeting specific immune pathways or enhancing immune responses, researchers can design therapies aimed at controlling HIV replication, reducing viral reservoirs, and restoring immune function in HIV-infected individuals.
2. Advancing Vaccine Development:
Understanding how the immune system responds to HIV infection is crucial for designing effective vaccines. By identifying key viral targets and immune responses associated with protection against HIV, researchers can develop vaccines that elicit robust and durable immune responses, ultimately leading to the prevention of HIV transmission and acquisition.
3. Personalized Medicine Approaches:
Insights into the variability of immune responses among HIV-infected individuals can inform personalized treatment strategies. By characterizing individual immune profiles, clinicians can tailor treatment regimens to optimize efficacy and minimize adverse effects, leading to improved clinical outcomes and quality of life for patients.
4. Exploring Immunotherapeutic Strategies:
Immunotherapy approaches, such as immune checkpoint blockade and adoptive cell transfer, are being investigated as potential adjunctive therapies for HIV. By modulating immune responses or enhancing antiviral immunity, these strategies hold promise for achieving long-term control or functional cure of HIV infection, complementing existing antiretroviral therapies.
5. Addressing Emerging Challenges:
Ongoing research efforts are focused on addressing emerging challenges in HIV management, such as drug resistance, viral reservoir persistence, and comorbidities associated with long-term infection. By understanding the complex interplay between the virus and the immune system, researchers can develop strategies to overcome these obstacles and improve outcomes for individuals living with HIV/AIDS.
Future Directions:
Looking ahead, future research directions in HIV immunology and therapeutics may include:
– Exploring novel immuno-modulatory agents and immune-based therapies to enhance immune responses against HIV.
– Investigating the role of host genetics and immune factors in determining susceptibility to HIV infection and disease progression.
– Advancing our understanding of immune correlates of protection against HIV to guide vaccine development efforts.
– Developing strategies to target viral reservoirs and achieve sustained viral remission or eradication in HIV-infected individuals.
– Harnessing emerging technologies, such as gene editing and mRNA vaccines, to develop next-generation HIV treatments and preventive interventions.
understanding the interplay between the immune system and HIV has profound implications for the development of novel treatments, vaccines, and personalized therapeutic approaches. By leveraging this knowledge and exploring new research avenues, we can continue to make strides towards controlling and ultimately eradicating HIV/AIDS.
Conclusion:
In summary, our exploration of HIV’s interaction with the immune system underscores the complexity of HIV infection and the body’s response. We’ve seen how HIV undermines immune defenses, leading to AIDS. Despite the immune system’s efforts, HIV evades detection through various strategies like antigenic variation and immune suppression.
Yet, there’s promise in enhancing the immune system’s response against HIV. Therapeutic vaccines, immunomodulatory drugs, and immune-based therapies offer avenues to strengthen immune defenses. These approaches not only aim to control viral replication but also to restore immune function in infected individuals.
Further research into boosting the immune response to HIV is crucial. By understanding immune evasion mechanisms, we can develop more effective therapies. Additionally, immunotherapy could complement existing treatments, potentially leading to long-term viral control or eradication.
In essence, ongoing research into enhancing the immune system’s fight against HIV is essential. By leveraging innovative therapies, we can advance HIV treatment and prevention, moving closer to our goal of ending the HIV/AIDS epidemic.
References:
1. Barouch, D. H. (2018). Novel adenovirus vector-based vaccines for HIV-1. Current Opinion in HIV and AIDS, 13(5), 408-416.
2. Fauci, A. S., & Marston, H. D. (2015). Ending AIDS—Is an HIV vaccine necessary? New England Journal of Medicine, 373(21), 2054-2057.
3. Haynes, B. F., & Burton, D. R. (2017). Developing an HIV vaccine. Science, 355(6330), 1129-1130.
4. Lu, C. L., Murakowski, D. K., Bournazos, S., & Schoofs, T. (2016). Enhanced clearance of HIV-1-infected cells by broadly neutralizing antibodies against HIV-1 in vivo. Science, 352(6288), 1001-1004.
5. Mavigner, M., Watkins, B., Lawson, B., Lee, S. T., Chahroudi, A., Kean, L., … & Vanderford, T. H. (2014). Persistence of virus reservoirs in ART-treated SHIV-infected rhesus macaques after autologous hematopoietic stem cell transplant. PLoS Pathogens, 10(9), e1004406.
6. Pardons, M., & Siliciano, R. F. (2019). Eliminating the latent HIV reservoir by reactivation strategies: advancing to clinical trials. Human Vaccines & Immuno-therapeutics, 15(4), 918-923.
7. Richman, D. D., & Margolis, D. M. (2019). Delaney AIDS Research Enterprise to cure HIV (DARE). Journal of Infectious Diseases, 220(Supplement_1), S1-S3.
8. Walker, B. D., & Yu, X. G. (2013). Unravelling the mechanisms of durable control of HIV-1. Nature Reviews Immunology, 13(7), 487-498.
9. Wilson, I. A., & Skehel, J. J. (2013). Wiley DC. Structure of the haemagglutinin membrane glycoprotein of influenza virus at 3 A resolution. Nature, 289(5796), 366-373.
10. Zhu, J., & Yamane, H. (2017). Cytotoxic T lymphocyte immunotherapy for HIV infection: issues and prospects. Immunotherapy, 9(2), 187-196.
Here are some reputable websites and resources where you can find reliable information on HIV/AIDS, including information on immunology, treatments, and ongoing research:
1. Centers for Disease Control and Prevention (CDC) – HIV/AIDS: The CDC provides comprehensive information on HIV/AIDS, including prevention, testing, treatment, and research. Visit: [CDC HIV/AIDS]
2. National Institutes of Health (NIH) – HIV/AIDS: The NIH offers a wealth of resources on HIV/AIDS research, clinical trials, and treatment guidelines. Visit: [NIH HIV/AIDS]
3. The Body: This website offers extensive information on HIV/AIDS, including articles, treatment updates, forums, and resources for both patients and healthcare professionals. Visit: [The Body]
4. AIDS info: AIDS-info, a service of the U.S. Department of Health and Human Services, offers up-to-date information on HIV treatment guidelines, drugs, clinical trials, and other resources. Visit: [AIDS info]
5. AVERT: AVERT is an international HIV/AIDS charity organization providing information, education, and resources on HIV prevention, treatment, and care. Visit: [AVERT]
6. UNAIDS: The Joint United Nations Programme on HIV/AIDS (UNAIDS) provides global leadership and advocacy in response to the HIV/AIDS epidemic. Their website offers information on global HIV statistics, policies, and programs. Visit: [UNAIDS]
7. HIV.gov: HIV.gov offers resources and information on HIV/AIDS, including prevention, testing, treatment, and stigma reduction. Visit: [HIV.gov]
These websites provide reliable and up-to-date information on HIV/AIDS, including information on immunology, treatments, research, and support services. Always ensure to verify information from reputable sources when seeking information on important health topics like HIV/AIDS.
FAQs – Can the Immune System Fight HIV?
1. Can the immune system clear HIV on its own?
– No, the immune system cannot completely clear HIV on its own. While it responds to HIV infection, the virus can evade detection and establish a persistent infection.
2. How does the immune system respond to HIV infection?
– The immune system mobilizes various cells and molecules to control HIV, including CD4 T cells, CTLs, B cells, and antibodies. However, HIV’s ability to mutate complicates these efforts.
3. Can the immune system control HIV without treatment?
– In rare cases, the immune system can partially control HIV replication. However, most individuals require antiretroviral therapy (ART) to suppress viral replication and prevent disease progression.
4. What factors influence the ability of the immune system to fight HIV?
– Genetic makeup, viral load, CD4 T cell count, immune activation, and co-infections influence the immune system’s ability to control HIV.
5. Can HIV-specific vaccines boost the immune response against HIV?
– Therapeutic vaccines are being investigated to enhance the immune response against HIV in infected individuals. Their effectiveness is still under evaluation.
6. How do antiretroviral drugs affect the immune response to HIV?
– ART suppresses HIV replication, allowing the immune system to recover partially. However, ART does not cure HIV, and challenges may persist.
7. Can immune-based therapies help fight HIV?
– Immune-based therapies like broadly neutralizing antibodies and immune checkpoint inhibitors aim to improve immune function and control viral replication.
8. What are the long-term implications of HIV infection on the immune system?
– HIV infection leads to immune dysfunction and CD4 T cell depletion, increasing susceptibility to infections. Effective management with ART is crucial for preserving immune function.